A Closer Look At Her Health Journey: A Journey from Crisis to Resilience
A Closer Look At Her Health Journey: A Journey from Crisis to Resilience
Prolonged autoimmune disorder, a journey marked by fatigue, misdiagnosis, and relentless resilience—this is the story unfolding behind the public face of a woman whose health journey has become a powerful testament to perseverance, medical inquiry, and the importance of patient advocacy. Her struggle began in early adulthood, when recurring fatigue, joint pain, and gastrointestinal distress defied easy explanation, leading to years of trial and error with conventional treatments that provided only temporary relief. What followed was not a straight path to diagnosis, but a deeper, more arduous expedition into the unknown—one that eventually revealed a complex autoimmune condition with systemic consequences.
Through medical records, personal testimony, and expert insights, this article unpacks the layers of her experience, highlighting not just medical milestones, but the human cost and ultimate transformation tied to her recovery.
The Early Days: Misdiagnosis and Frustration
From the outset, symptoms were persistent yet vague: persistent fatigue that worsened with exertion, intermittent fevers, and severe digestive disturbances. Early visits to internal medicine specialists yielded inconsistent diagnoses—fibromyalgia, irritable bowel syndrome, even anxiety disorders—each failing to account for the full clinical picture.At a pivotal moment, a persistent high-titer rheumatoid factor and positive antinuclear antibody (ANA) test prompted further testing, revealing autoantibodies suggestive of systemic lupus erythematosus (SLE), but diagnosis remained elusive. “I felt like a mystery box of symptoms,” she recalled in an interview, “with doctors patching together clues no one saw as part of one larger condition.” This diagnostic limbo lasted years, during which financial strain, emotional instability, and declining physical function took a passage-bearing toll.
The Toll of Uncertainty
Living without a confirmed diagnosis exacted profound personal costs.“There were months where I couldn’t work, care for family, or even come out of bed,” she shared. The constant cycle of undiagnosed pain and inflammation eroded self-trust and mental well-being. Social outings became rare; trust in medical systems wavered.
Challenging socioeconomic barriers—limited access to specialized care, insurance hurdles, fragmented specialist referrals—only deepened frustration. Yet, rather than resign herself to perpetual diagnosis, she pursued alternative avenances: patient-led advocacy groups, online medical forums, and direct dialogue with rheumatologists who specialized in complex autoimmune cases.
Unraveling the Mystery: The Journey to Diagnosis
The breakthrough arrived not from a single test or clinical hunch, but from persistent collaboration between the patient and a multidisciplinary team.In late-stage evaluation, advanced serological panels detected anti-dsDNA and anti-Smith antibodies—key markers for lupus—alongside a pattern of complement protein depletion consistent with active disease. A definitive diagnosis followed, grounded simultaneously in immunofluorescence testing, imaging, and longitudinal symptom tracking. “It felt like seeing a map where I’d only been walking blind,” she reflected.
Her team implemented a tailored treatment protocol combining low-dose corticosteroids, hydroxychloroquine, and lifestyle interventions, supported by regular monitoring via telehealth and in-person follow-ups. While remission remains a dynamic goal rather than a certainty, measurable improvements in energy levels, pain scores, and inflammatory markers underscored meaningful progress.
Beyond Lab Results: The Holistic Treatment Approach
The clinical management extended beyond pharmaceuticals.Recognizing the autoimmune condition’s multifaceted impact, her care plan incorporated nutritional therapy, stress reduction techniques, and gentle physiotherapy. Omega-3 fatty acids and vitamin D supplementation supported immune modulation, while mindfulness practices reduced anxiety spikes linked to symptom flares. Importantly, she engaged in shared decision-making with clinicians, fostering a partnership grounded in trust and transparency.
“They didn’t just prescribe drugs—they listened,” she noted. This holistic framework emphasized patient agency, integrating behavioral science and integrative medicine as complementary tools in managing chronic illness.
Navigating Long-Term Management and Relapse
Life post-diagnosis brought persistent vigilance.Autoimmune diseases are inherently dynamic, requiring careful adjustment of regimens as triggers emerge—whether environmental (infections, UV exposure), physiological (menstrual cycles), or psychological. Relapses tested both physical endurance and emotional resilience. During particularly severe flare-ups, marked by widespread gigionitis, meningitis-like headaches, and acute fatigue, daily routines shifted dramatically.
Strict rest, reinforced immunosuppression, and frequent medical check-ins became norms. Yet, each relapse also deepened understanding, enabling preemptive adjustments. “It taught me to anticipate, adapt, and advocate for myself in ways I never imagined,” she said.
Blood work, symptom diaries, and open communication with her care team formed a proactive foundation, turning unpredictability into a manageable rhythm.
The Power of Advocacy and Patient Education
Her journey transformed from a personal battle into a public mission. No longer passive in clinical encounters, she now leads workshops and speaks at health conferences, emphasizing the critical value of patient-reported outcomes and sustained dialogue with providers.Drawing from her experience, she promotes early awareness of subtle, overlapping symptoms—especially among women, who statistically face higher risks for autoimmune diseases. Educational resources she co-developed highlight key warning signs: persistent fatigue unresponsive to rest, unexplained fevers, sudden rashes, and gastrointestinal crises that defy routine treatment. “Awareness is power,” she asserts.
“If we spot the red flags earlier, we catch the disease before it progresses.” Her advocacy bridges gaps between biomedical perspectives and lived reality, urging both patients and providers to see beyond isolated symptoms to the whole person.
A Blueprint for Resilience and Hope
This woman’s health journey exemplifies the convergence of science, perseverance, and human determination. From years of confusion and isolation to a diagnosed, managed condition—one shaped by both medical precision and personal courage—her story reveals core truths about chronic illness: there is no universal cure, but strategies exist to reclaim agency and quality of life.The path was neither linear nor easy, yet it yielded measurable relief, deeper medical understanding, and a renewed sense of purpose. Her experience illustrates how patient engagement transforms clinical outcomes; when individuals become active partners in their care, treatment becomes more responsive and holistic. Moreover, her advocacy reshapes conversations around autoimmune diseases, particularly as gender disparities in diagnosis and treatment persist.
Ultimately, her journey is not merely a personal narrative, but a compelling case study in resilience—one that inspires hope, demands systemic attention, and reaffirms the power of never giving up, even when the road is uncertain.




Related Post
Understanding Gloria Borger’s Illness: A Raw and Resilient Journey Through America’s Pressing Health Challenges
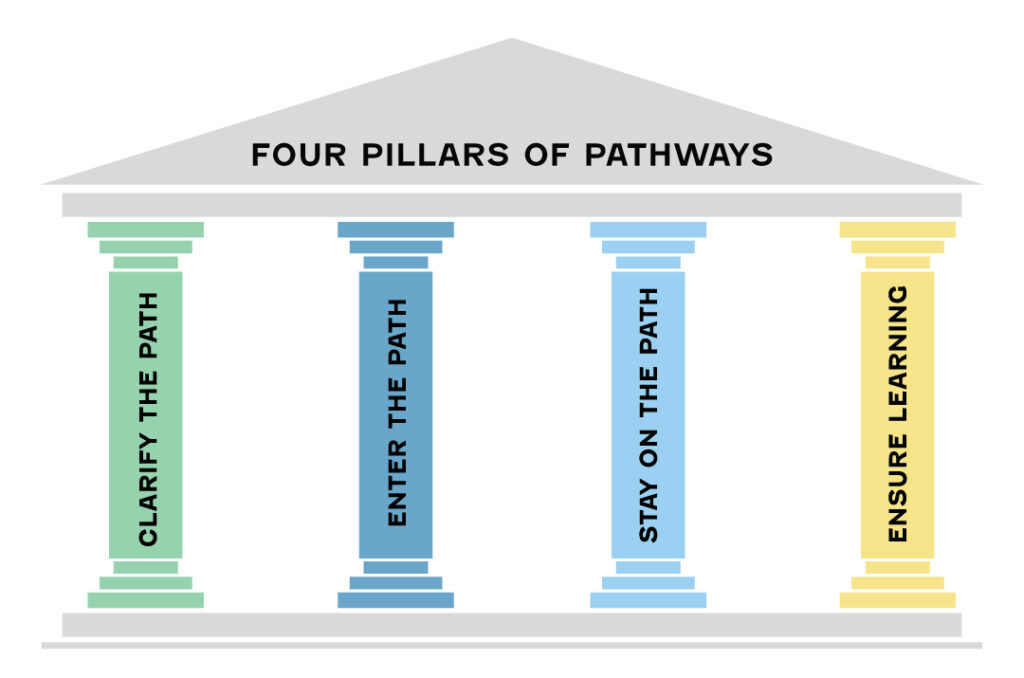
Florida Colleges: Pathways to Opportunity, Innovation, and Success

Hapy Hip Number Two: The Rise, Reinvention, and Reckoning of Tim Schmidt, Known as Hppy Hippie Inside

Dámaso E. Uriburu Memorias: The First Architect of Modern Argentine Political Strategy

