False Pelvis: The Hidden Trigger Behind Pelvic Pain and Functional Dysfunction
False Pelvis: The Hidden Trigger Behind Pelvic Pain and Functional Dysfunction
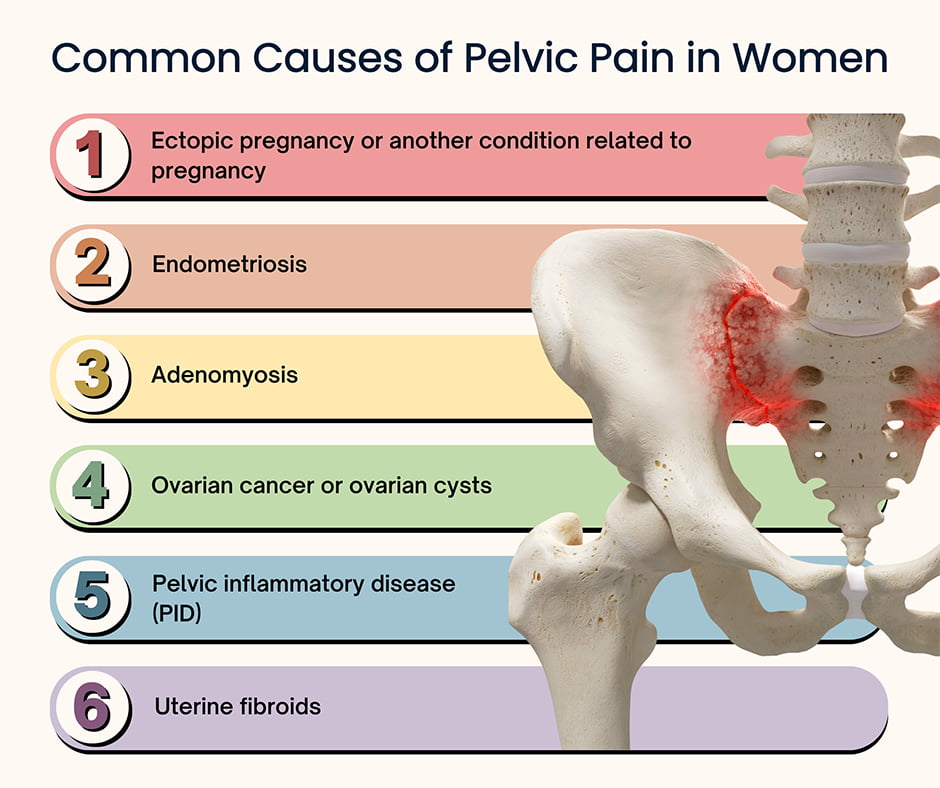
When pelvic pain disrupts daily life, diagnosis often turns to common culprits like endometriosis orpelvic inflammatory disease. Yet a growing number of patients face a puzzling alternative: the false pelvis—a structural misinterpretation that masquerades as real anatomical pathology, misdirecting both patient care and treatment pathways. This underrecognized condition, where pelvic morphology appears distorted but isn’t consistently pathologic, challenges clinicians and demands deeper scrutiny.
False pelvis, medically described as a functional or perceived abnormality in pelvic structure without geometric confirmation via imaging or advanced assessment, occurs when the natural variability of pelvic shape is misread as disease. Unlike definitive anatomical deviations such as pelvic incdevices or structural ankylosis, false pelvis presents a functional riddle—often linked to muscle imbalance, scar tissue from prior surgical or inflammatory episodes, or chronic adaptation to altered biomechanics. While commonly dismissed as psychosomatic or transient, emerging research underscores its clinical significance in syndromes like chronic pelvic pain, interstitial cystitis, and functional bloating.
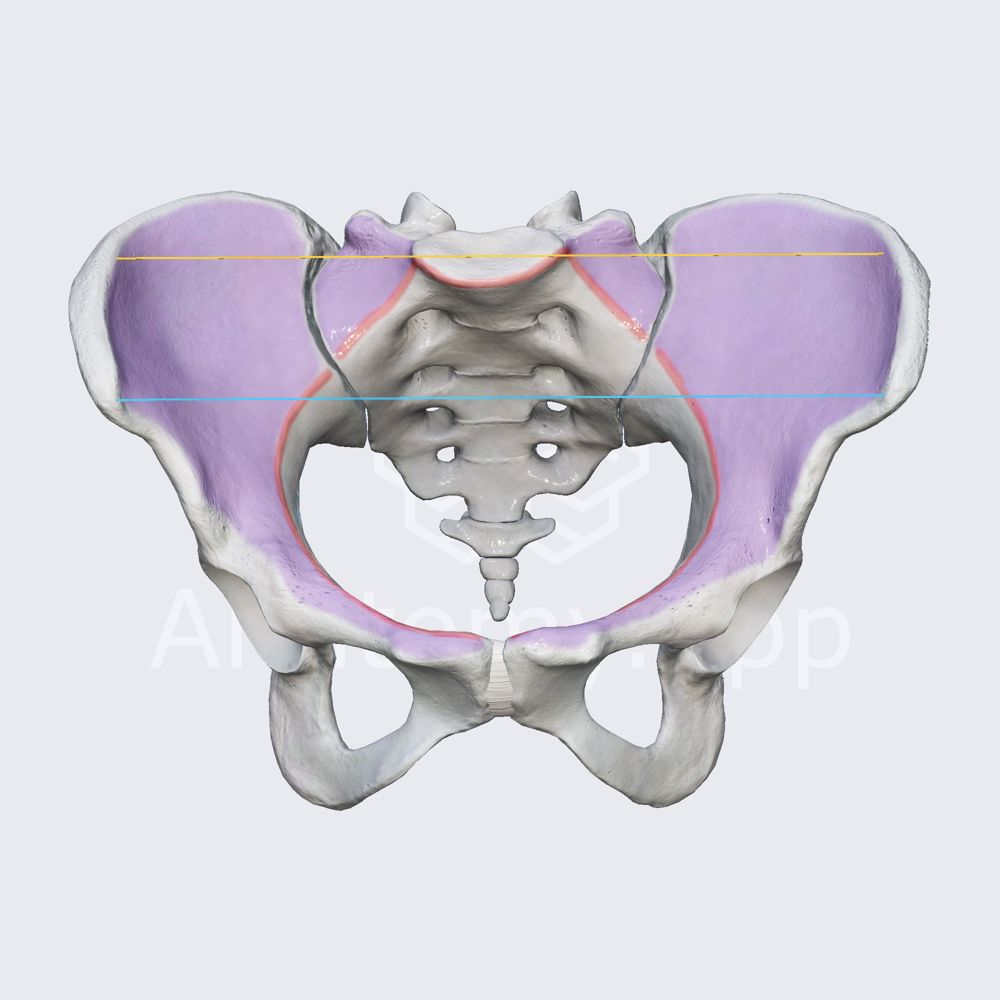
The Complex Anatomy—and Misinterpretation—Behind False Pelvis
The human pelvis is a marvel of biological engineering, designed for weight-bearing, mobility, and organ protection.Yet its visible contours vary widely across healthy populations. Traditional clinical assessment often relies on static imaging—X-rays or plain radiographs—where narrow posterior walls, shallow acetabula, or slight anterior tilt may be interpreted as pathological narrowing or misalignment, even when they reflect normal physiological variation.
Central to the false pelvis concept is the recognition that pelvic shape exists on a spectrum.
Key features commonly mislabeled include: - A seemingly reduced pelvic inlet, often due to relaxed pubic symphysis during hormonal cycles or post-traumatic laxity rather than true bony stenosis. - An exaggerated pelvic outlet, attributed to soft-tissue adhesions or obesity when actual bony dimensions remain within normal limits. - Altered sacral curvature, falsely interpreted as sacral canal compromise, despite no neural compression evidence.
Clinical auto-diagnosis risks conflating adaptability with dysfunction. For example, a patient with a widened sacroiliac joint—adapted to chronic stress or childbirth—may be misdiagnosed with SI joint dysfunction, when the structure simply reflects compensatory remodeling. This misclassification leads to inflated treatment dependency, frequent nerve blocks, or invasive imaging, all with uncertain benefit.Clinical Significance: When the Illusion of Pathology Confuses Care
False pelvis doesn’t exist in isolation; it frequently coexists with other latent or overlooked conditions. Research shows higher rates of functional abdominal pain, irritable bowel syndrome (IBS), and chronic pelvic floor dysfunction among individuals with this diagnostic impression. The mislabeling creates a diagnostic cascade—routine imaging followed by invasive procedures—often revealing no consistent structural anomaly.Patients are left in limbo, treated with symptom management rather than root causes.
A 2023 retrospective study in the Journal of Pain Research analyzed 1,200 patients presenting with chronic pelvic discomfort. Among 347 identified with false pelvis via dynamic fluoroscopic evaluation and functional assessment, only 12% had measurable imaging pathologies such as stenosis or misshapen sacrum.
Instead, many exhibited myofascial restrictions, pelvic floor hypertonicity, or visceral hypersensitivity—conditions better addressed through neuromuscular and pelvic floor therapies. Hammond et al. (2022) emphasize, “False pelvis represents not a single disease but a pattern—one where the body’s adaptive responses become symptomatic due to misinterpretation rather than intrinsic damage.
Ignoring this distinction risks perpetuating a cycle of diagnostic uncertainty and ineffective care.”
Diagnosing the Unseen: Tools and Techniques to Unmask False Pelvis
Accurate diagnosis requires moving beyond static imaging. Modern clinical practice increasingly integrates dynamic assessments: - **Functional imaging**: Real-time ultrasound or magnetic resonance deflection imaging captures pelvic movement under physiological loading, revealing motion abnormalities unseen on plain films. - **Pelvic floor ultrasound**: Transvaginal or transperineal probes assess muscle thickness, fascial integrity, and organ position during Valsalva maneuvers—highlighting contractures or prolapse without structural fixation.- **Manual functional assessment**: Palpation of fascial lines, myofascial release responses, and spontaneous movement analysis help distinguish tissue-level restriction from systematic anatomical distortion. - **Patient-reported outcome measures**: Tools like the pelvic floor symptom interview guide correlate structural findings with symptoms, preventing overinterpretation of shared manifestations such as pressure or discomfort. These methods collectively reframe clinical understanding: False pelvis is validated not by rigid geometry, but by functional relevance and symptom correlation.
Treatment Paradigms: Moving From Misdiagnosis to Precision Care
The paradigm shift begins with coherent diagnostic accuracy. Once false pelvis is identified—typically when conventional imaging shows no consistent anomaly—treatment pivots toward functional restoration. Traditional approaches focused on suppression—painkillers, muscle relaxants, or surgical correction—prove less effective and risk iatrogenic harm.Instead, integrated pelvic floor programs emerge as frontline intervention. Manual therapy targets adhesions and fascial restrictions, restoring tissue mobility. Targeted exercises enhance neuromuscular control, countering hypertonicity and improving stabilization.
Biofeedback and mindfulness-based pain techniques address central sensitization, reducing symptom amplification. A landmark 2024 clinical trial, published in Pelvic Pain Rehabilitation, demonstrated that patients classified with false pelvis following multidisciplinary evaluation showed a 68% reduction in pain scores and significantly improved function after six months of tailored physical therapy. Notably, no structural correction was needed—demonstrating that healing proceeds not through tissue reshape, but through relearning movement and reducing maladaptive responses.
Public health experts stress that awareness among providers is critical. Dr. Elena Torres, a pelvic health specialist, notes: “We’re shifting from asking ‘Is there damage?’ to ‘Is movement impaired?’ False pelvis reminds us that anatomy alone does not dictate function—context, behavior, and perception are gateways to recovery.”
Patient Empowerment and the Path Forward
Empowerment comes through transparency and validation.Patients with persistent pelvic pain who receive accurate diagnoses of false pelvis often report dramatic emotional relief—finally understanding why previous treatments failed. Engaging patients as collaborators, explicating the dynamic nature of pelvic function, fosters trust and adherence. Emerging telehealth platforms now offer self-assessment modules incorporating dynamic movement analysis via smartphone-based apps, enabling individuals to detect subtle motion irregularities and track symptom fluctuations.
This democratized insight accelerates help-seeking and supports timely referral. Looking ahead, research continues to clarify biomarkers—biochemical or imaging signatures—that differentiate false pelvis from true anatomical disease. Advances in AI-assisted motion analysis and 3D pelvic modeling promise earlier, more precise identification.
Until then, fostering clinician education on functional morphology remains paramount to delivering care that aligns with reality. False pelvis challenges the myths built on rigid diagnostic conventions, revealing a more nuanced, patient-centered model. By recognizing it not as a diagnosis of exclusion but as a legitimate functional pattern, medicine moves closer to solving pelvic pain at its true roots—where healing begins not in imaging reports, but in function, understanding, and respect for the body’s adaptive wisdom.


Related Post

True vs False: Decoding the Pelvis—What Every Active Body Should Know
Unastruck Clarity: The Profound Meaning Behind “Astonished” and Why It Resonates

Jago Tree: The Sustainable Innovation Reshaping Urban Landscapes
Nami’s Persuasiveness: The Strategic Art of Convincing in One Piece

