Frozen Shoulder Unlocked: Understanding ICD-10 Freezing Shoulder with Precision and Depth
Frozen Shoulder Unlocked: Understanding ICD-10 Freezing Shoulder with Precision and Depth
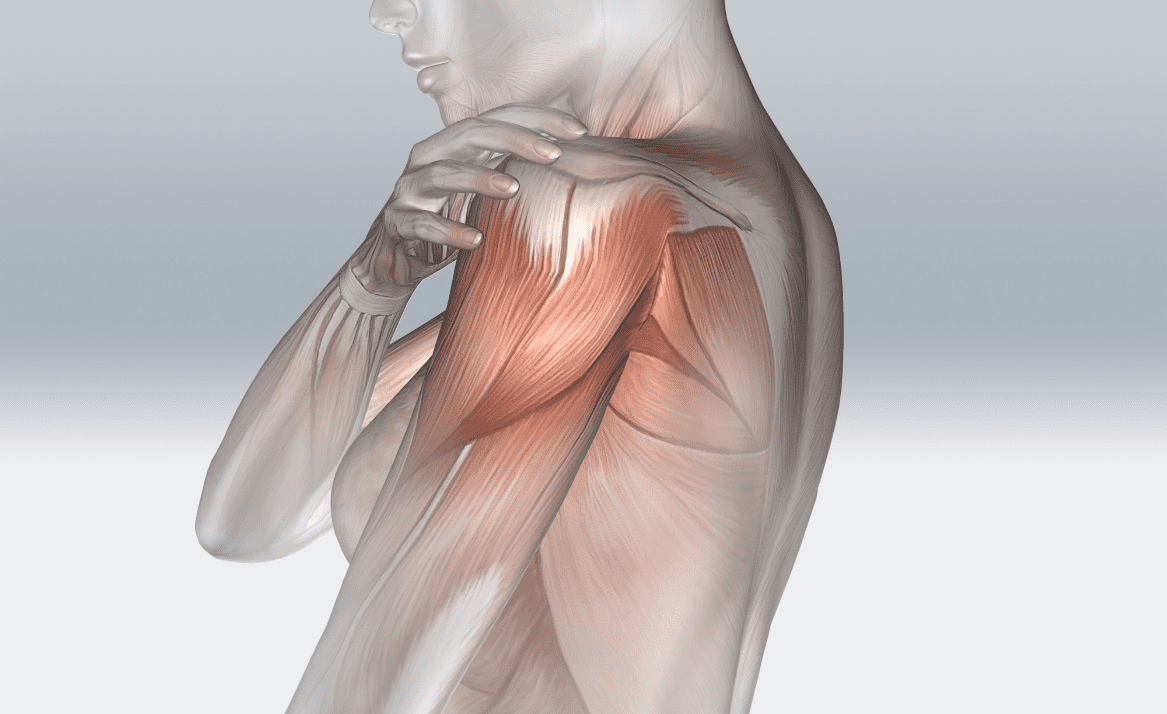
Frozen shoulder, clinically known as adhesive capsulitis, is a disabling condition marked by progressive stiffness and pain in the shoulder joint, often limiting daily movement and independence. Affecting approximately 2–5% of the general population, this syndrome commonly impacts adults aged 40 to 65, though recent data show rising incidence in younger adults and even pediatric cases. The clinical picture unfolds in stages—early pain followed by gradual loss of range of motion, culminating in near-complete immobilization.
Crucially, accurate diagnosis via ICD-10 coding ensures appropriate treatment pathways, making understanding of its ICD classification essential for clinicians and patients alike.
Decoding ICD-10 Classification for Frozen Shoulder
The International Classification of Diseases, Tenth Revision (ICD-10), maintained by the World Health Organization, serves as the global standard for medical billing, epidemiology, and clinical documentation. For frozen shoulder, the designated ICD-10 code is S32.5 — defined specifically as “Adhesive capsulitis of the shoulder.” This precise classification reflects not only the anatomical site but also the pathological hallmark: fibrosis and thickening of the joint capsule, resulting in restricted mobility.According to clinical guidelines, ICD-10 coding demands specificity. S32.5 distinguishes frozen shoulder from other causes of shoulder dysfunction such as rotator cuff tears or tennis elbow, which carry separate codes (e.g., S32.81). The panel defining S32.5 emphasizes: “Stiffness without traumatic injury, with documented limitation of internal rotation exceeding 70 degrees in advanced stages.” This specificity prevents misdiagnosis, enabling healthcare systems to track incidence, allocate resources, and evaluate treatment efficacy.
“Precision in coding transforms patient care,” notes Dr. Elena Rostova, a rheumatologist at the National Shoulder Institute. “Without ICD-10 S32.5, the complexity of frozen shoulder—its insidious onset, gradual progression, and variable response to therapy—gets lost in broader diagnoses like ‘shoulder pain.’”
Staged Progression: The Clinical Journey of Frozen Shoulder
Frozen shoulder rarely strikes suddenly; rather, it evolves through three objective stages, each with distinct clinical features and patient experiences.**Stage 1: Freezing (Pain-Prone Phase)** Characterized by deep, aching pain localized primarily on the posterior shoulder, this phase typically lasts six to nine months. Patients often describe sharp discomfort during arm movements, with gradual but persistent loss of motion. “At first, I couldn’t comb my hair or reach behind my back,” recalls Maria G., a 52-year-old marketing executive diagnosed in year three.
MRI evidence confirms early inflammatory changes and capsular thickening, though imaging alone cannot confirm diagnosis without clinical correlation. **Stage 2: Frozen (Adhesive Phase)** During this two- to six-month period, pain may lessen in intensity, but stiffness becomes entrenched. Range of motion drops significantly—especially in abduction and external rotation—leaving patients unable to perform routine tasks.
“It’s like my shoulder has moved into a permanent burial,” says James T., a 60-year-old carpenter. While pain decreases, quality of life deteriorates rapidly due to functional limitations. **Stage 3: Thawing (Recovery Phase)** Lasting up to two years, this stage sees gradual improvement as joint flexibility slowly returns.
Though frustrating, progress remains slow and nonlinear. Adherence to structured physical rehabilitation becomes critical, as overzealous movement risks re-injury. “I thought I’d never swing a pickleball paddle again,” James adds, “but with consistent therapy, meaning recovered about 60% of my motion.” Understanding these phases helps both patients and providers differentiate frozen shoulder from conditions like shoulder impingement or osteoarthritis—each requiring distinct therapeutic approaches.
Beyond S32.5: Usage, Limitations, and Clinical Integration
While S32.5 represents the ICD-10 cornerstone for frozen shoulder, clinical practice demands attention to contextual coding. Co-morbidities such as diabetic neuropathy (E11.9), cervical spondylosis (M54.5), or post-surgical fibrosis (Z56.89) may coexist and require parallel documentation to capture the full clinical picture. Additionally, ‘unspecified shoulder stiffness’ (otherwise healthy population – S02.9) is not ICD-10 compatible, underscoring the necessity of precise staging.ICD-10 coding supports epidemiological surveillance—tracking trends tied to aging populations, sedentary lifestyles, or metabolic disorders—enabling public health initiatives targeting prevention. Meanwhile, accurate diagnosis via S32.5 ensures appropriate utilization of imaging, physical therapy, and sometimes pharmacologic or interventional treatments, minimizing unnecessary expenses. “Every misscoded capsule is a missed opportunity,” caution residue specialist Dr.
Amir Chen. “Without the right code, a patient’s struggle remains invisible in registries, and funding for treatment stalls.”
The Path Forward: Rehabilitation, Prevention, and Smart Diagnosis
Frozen shoulder remains a diagnosis of exclusion and clinical judgment, where imaging augments—not replaces—historical and physical evaluation. Standard therapy blends passive mobilization, active rehabilitation, and in select cases, corticosteroid injections or arthroscopic capsular release.Early intervention during the freezing phase correlates strongly with better recovery, emphasizing timely referral. Prevention hinges on awareness. Stretching routines, posture correction, and early treatment of rotator cuff disorders can reduce risk.
For athletes, coaches and physical therapists increasingly integrate shoulder mobility protocols into training regimens. With ICD-10 S32.5 firmly establishing a common language, stakeholders—from patients to insurers—operate on the same diagnostic footing. This clarity propels precision medicine, optimized care pathways, and data-driven research.
Frozen shoulder, once shrouded in ambiguity, emerges in its full clinical reality—mapped, measurable, and manageable.



Related Post

Emily Wilson’s Iliad: Get Your PDF Copy for Unprecedented Access to Homer’s Epic

Ufc Bmf Belt

What Time Do The Tigers Play Today? The Rhythm of Rest and Resilience

Mexicanos Halal: The Rising潮 of Ethical Meat in a Sew 올te Cult Scene

