Mastering Tidal Volume Calculation: The Key to Precise Respiratory Assessment
Mastering Tidal Volume Calculation: The Key to Precise Respiratory Assessment
Tidal volume stands as one of the most fundamental yet critical parameters in respiratory physiology, reflecting the amount of air inhaled or exhaled during a normal breath. Accurately calculating tidal volume empowers clinicians, researchers, and respiratory therapists to evaluate lung function, monitor disease progression, and tailor ventilation strategies with precision. Whether assessing healthy individuals or patients on mechanical ventilation, understanding the methods and mathematics behind tidal volume enables timely, evidence-based clinical decisions that can save lives.
This article unpacks the science, formulas, real-world applications, and evolving techniques in tidal volume calculation—revealing why it remains indispensable in modern respiratory medicine.
Tidal volume is defined as the volume of air moved into or out of the lungs during a single, average breath under resting conditions. For a healthy adult at rest, this typically ranges between 500 and 600 milliliters (mL), with an average of approximately 500 mL—but values vary significantly based on age, sex, body size, and physical condition. Even subtle deviations from expected volumes can signal critical respiratory compromise, making precise measurement essential.
As one pulmonary physiologist notes, “Tidal volume isn’t just a number; it’s a dynamic window into pulmonary mechanics and systemic health.”
Understanding the Core Formula: How Tidal Volume is Measured
At its mathematical heart, tidal volume (TV) is calculated using a straightforward volumetric equation: TV equals the total air moved per breath minus or plus respiratory variations, derived from volume changes before and after a breath. The most direct measurement comes from direct volumetric assessment, typically via body plethysmography—a gold-standard respiratory analysis technique. This method captures the full air flow and volume changes in a sealed chamber while the subject breathes normally, allowing clinicians to compute the exact volume of air exchanged per cycle.
A simpler clinical equivalent comes from spirometry, where tidal volume is derived indirectly using critical derived values.
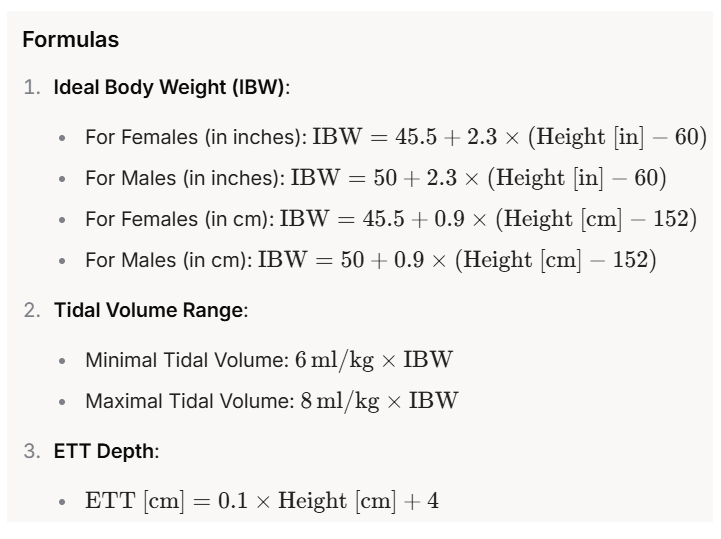
While spirometers primarily measure airflow and total lung capacity, tidal volume can be calculated using the basic breathing equation when minute ventilation (MF) and respiratory rate (RR) are known:
TV = (Minute Ventilation) / (Respiratory Rate)Minute ventilation itself is the product of tidal volume and breathing frequency, making spirometry data—often collected during routine pulmonary function tests—vital for estimating TV in practical settings. Though indirect, this formula provides reliable estimates when total lung capacity and respiratory rate are well-documented through standard pulmonary function tests.
Direct Measurement: The Body Plethysmography Technique
For maximal accuracy, direct measurement via body plethysmography remains the benchmark. In this non-invasive method, patients sit or lie inside an airtight chamber.
Precise physical assessment monitors changes in thoracic volume—via pressure and displacement—during full inspiration and expiration, capturing minute volume (MV) and expiratory reserve volume (ERV) to isolate tidal volume with exceptional fidelity. The calculation remains: TV = MV – (ERV + RES – RV), though standards simplify this based on impedance plethysmography or flow-volume loops for clinical workflows.
This technique excels in research and intensive care, where subtle airway obstruction or restrictive lung disease must be detected early. “Plethysmography offers an unmatched window into lung function, revealing details airflow alone cannot,” explains a clinical respiratory specialist.
“It captures the true mechanics of breathing, crucial for diagnosing conditions like COPD, asthma, or interstitial lung disease.”
Clinical Applications That Depend on Precision Tidal Volume Calculations
Tidal volume measurement is foundational across multiple domains of respiratory care, directly influencing diagnosis, treatment, and monitoring.
- Mechanical Ventilation Management: In intensive care units, mechanical ventilation relies on accurate tidal volume delivery to avoid ventilator-induced lung injury. “Using incorrect TV settings—even by a few milliliters—can worsen inflammation or collapse alveoli,” warns a critical care expert. Protocols emphasize “lung-protective ventilation,” using TTV (tidal volume therapy) strategies targeting 4–8 mL/kg predicted body weight in ARDS patients.
- Pediatric and Neonatal Care: In infants and children, tidal volumes are fractionally higher per kilogram, making age-specific calculations vital.
Preterm neonates, with underdeveloped lungs, require careful TV adjustments to prevent atelectasis or hyperinflation.
- Diagnosis and Monitoring of Lung Diseases: Chronic conditions such as COPD and asthma involve altered airflow dynamics and reduced TV due to airway obstruction. Serial tidal volume assessments help track disease progression and response to bronchodilators.
Each application demands methodological rigor—whether direct plethysmography in advanced labs or spirometry-derived TV in primary care settings.
Emerging Techniques and Technological Innovations
Advancements in digital health and sensor technology are reshaping tidal volume measurement, shifting from exclusively clinical tools to portable, real-time systems.
Wearable devices now integrate flexible pressure sensors and acceleration-based flow monitoring to estimate tidal volume during daily activities. These systems enable continuous respiratory monitoring outside clinics, aiding rehabilitation and early detection of exacerbations in COPD or cystic fibrosis patients.
Machine learning algorithms further refine accuracy by adapting to individual breathing patterns and correcting for artifacts like speech or movement.
While promising, these innovations require validation against gold-standard methods. Nevertheless, they herald a new era where tidal volume becomes accessible, dynamic, and patient-specific—transforming preventive and personalized respiratory care.
Factors Influencing Accurate Tidal Volume Estimation
Multiple variables affect tidal volume reliability, demanding careful attention to protocol and physiology.
-Patient Cooperation: Incorrect breathing patterns—such as shallow or irregular breaths—distort volumetric measurements. Training patients and ensuring steady ventilation is key.
-Equipment Calibration: Spirometers and plethysmography chambers must be regularly calibrated to avoid systematic errors, especially in longitudinal studies.
-Physiological Variability: Factors including posture, fatigue, fever, and medications influence respiratory mechanics, necessitating standardized test conditions—sitting upright, fasting, and sampler times aligned with circadian rhythms.
Understanding these nuances ensures tidal volume data remains clinically meaningful across diverse settings.
Standardized Nursing and Clinical Protocols
To maintain consistency, respiratory care providers follow standardized protocols for tidal volume assessment.
These include:
Related Post

Perfusionist Salary: What To Expect in OSC Technology — What Recruits Really Want to Know
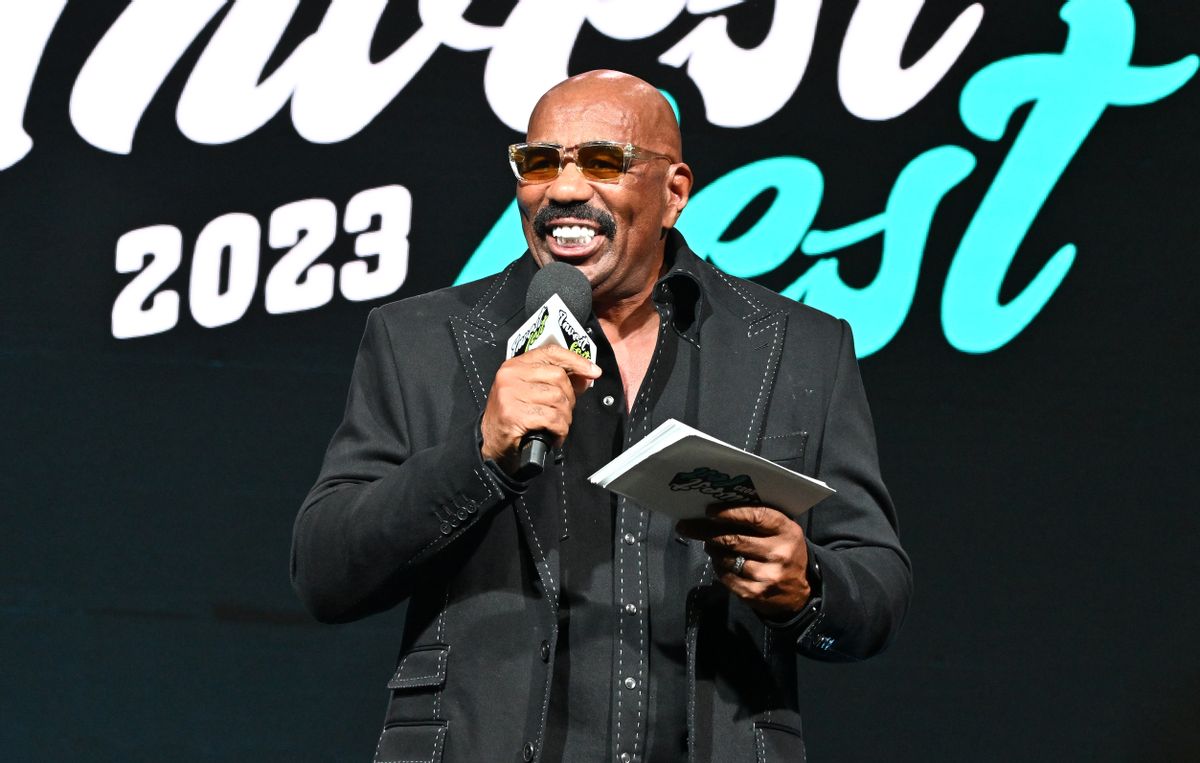
Is Steve Harvey Alive Or Dead? The Truth Behind The Rumors That Swept the Nation

Exploring The Life And Career Of James Maby: The Poet Who Wrote the Heart of a Nation

A Simple Guide to Personal Finance That Actually Works

