Severe Sepsis: The Silent Killer That Demands Immediate Action
Severe Sepsis: The Silent Killer That Demands Immediate Action
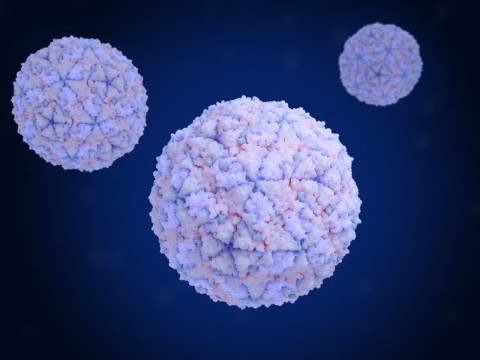
When the body’s immune system overreacts to infection, triggering a cascade of systemic inflammation, life-threatening complications can unfold in hours—severe sepsis being one of the most insidious. Defined by a combination of life-threatening organ dysfunction and a confirmed or suspected infection, severe sepsis affects millions globally every year, yet remains underrecognized until it reaches critical stages. Understanding its mechanisms, early warning signs, and treatment protocols is not just medical knowledge—it is a potential lifesaver.
At its core, severe sepsis arises when the immune system’s defensive response spirals into systemic dysregulation. This condition evolves from sepsis—a broader term that includes infection and systemic inflammatory response—but differs when organ system failure becomes evident. “Severe sepsis is not merely an infection with symptoms; it is the body’s flag signaling impending organ collapse,” notes Dr.
Elena Ruiz, critical care specialist at Johns Hopkins Hospital. “Without rapid intervention, mortality rises sharply, often outpacing diagnosis.”
The pathophysiology of severe sepsis centers on a cascade triggered by microbial invasion—bacteria, viruses, fungi, or parasites—sparking widespread inflammation. Cytokines surge uncontrollably, damaging endothelial linings of blood vessels and disrupting microcirculation.
The result: blood flow is compromised, tissues starved of oxygen, and vital organs begin to fail. Key organs affected include the lungs, kidneys, liver, and brain—each failure compounding the threat.
Organ dysfunction in severe sepsis manifests through distinct clinical criteria. The most widely used definition by the Surviving Sepsis Campaign enumerates—within 48 hours of infection—a diagnosis of severe sepsis if a patient shows:
- Hypotension requiring vasopressors to maintain mean arterial pressure above 65 mmHg, or lactate > 2 mmol/L despite fluid resuscitation.
- Acute renal failure defined as an acute rise in creatinine or reduced urine output.
- Respiratory distress, often indicated by hypoxemia or bilaterally abnormal lung findings on imaging.
- Altered mental status due to cerebral hypoxia or sepsis-associated encephalopathy.
The global burden of severe sepsis is staggering.
According to the World Health Organization, an estimated 11 million deaths annually stem from sepsis-related complications, with severe sepsis accounting for a significant proportion. In high-income countries, mortality ranges from 15% to 30%, but this soars in low-resource settings where diagnostic tools and timely antibiotics are scarce. Early identification remains paramount: studies show patients assessed within the first three hours of presentation have markedly improved outcomes.
But delay, even by hours, can transform a treatable infection into irreversible shock.
clinically, severe sepsis unfolds in stages, each demanding escalating intervention. The progression begins with systemic inflammatory response syndrome (SIRS), where fever, tachycardia, or tachypnea precede organ-specific failure. Clinicians rely on validated scoring systems—such as the quick SOFA (qSOFA)>>
- Sudden altered mentation (score ≥2 points)
- Respiratory rate ≥22 breaths/min
- Altered blood pressure or lactate ≥2 mmol/L
Diagnosis is a race against time.
Misdiagnosis or delayed diagnosis often stems from nonspecific early symptoms—fever without source, vague fatigue, or confusion. Point-of-care lactate testing has revolutionized assessment, offering rapid insight into tissue perfusion. Blood cultures, imaging, and serial organ scoring guide definitive management but cannot be delayed.
A 2022 study in Critical Care Medicine emphasized that “a missed hour in diagnosis for septic shock correlates directly with higher mortality—sever grain erosion in seconds.”
Treatment hinges on three pillars: rapid resuscitation, source control, and antimicrobial therapy. Resuscitation begins with aggressive fluid administration—typically crystalloids—while vasopressors stabilize blood pressure. Early vasopressor use, notably norepinephrine, limits cumulative organ injury.
However, identifying and eliminating the infection source—surgery, drainage, debridement—remains indispensable. “Without nailing the infection, even the best supportive care may fail,” warns Dr. Ruiz.
“Sepsis is the immune system fighting itself; its foe must be removed.”
Early antibiotic administration within one hour of suspicion is non-negotiable. Broad-spectrum coverage tailored to likely pathogens follows once culture results emerge. Overuse risks resistance, but delayed coverage endangers survival.
Guidelines from the Infectious Diseases Society stress a “broad-first, narrow-second” approach, balancing urgency with precision. Metabolic recovery, particularly lactate clearance, signals stabilization but requires sustained intensive care monitoring.
Advanced supportive measures—mechanical ventilation for ARDS, renal replacement therapy for acute kidney injury, and multi-organ support—complement core treatments but are interventions of last resort. Outcomes depend on both pathogen control and organ support, where timing and coordination determine fate.
Risk factors for developing severe sepsis include compromised immunity—from diabetes, cancer, or immunosuppressive therapy—as well as chronic conditions like chronic kidney disease or advanced age.
Post-surgical states, severe trauma, and indwelling devices (catheters, ventilation) further elevate risk. “Patients with comorbidities often present with atypical signs, masking early sepsis,” explains infectious disease specialist Dr. Amir Patel.
“We must maintain high vigilance, especially in ICU settings, where subtle shifts may herald disaster.”
Prevention remains the most underutilized weapon. Vaccination, timely resuscitation protocols, and early recognition training reduce incidence. In agriculture and healthcare, strict infection control limits nosocomial outbreaks.
Yet public awareness lags—most patients and even some providers remain unaware until crisis strikes. Campaigns like “Sepsis Syndrome Awareness” aim to bridge this gap, urging prompt recognition of fever, pain, confusion, and respiratory distress in any ill person.
In specialized ICUs, harsh but necessary protocols standardize care: sepsis bundles embedding rapid assessment, early antibiotics, and fluid resuscitation. These protocols have transformed survival—manufacturing a curtain between precarity and recovery.
Yet in resource-poor regions, such systems remain underdeveloped, deepening global inequities. Innovations in portable diagnostics and simplified treatment algorithms offer hope, democratizing access to timely care.
Severe sepsis is not an inevitable death sentence but a dynamic, treatable emergency—if spotted swiftly and acted upon decisively. Its complexity demands multidisciplinary vigilance, scientific rigor, and human compassion.
Every hour merged is a life quietly slipping away. For clinicians, it’s a call to relentless precision. For patients and families, it’s a plea for awareness.
Ultimately, severe sepsis teaches a harsh yet vital truth: in medicine’s race against time, knowledge is power—and hope is earned in the moments between diagnosis and treatment.



Related Post

Severe Sepsis A Comprehensive Guide: Understanding the Silent Killer Beneath Critical Illness
Unveiling the Mystery of Scott McGillivray’s Age – How Old Is the Media Strategist Behind the Brand?

Oscar Digital Print Mumbai: Where Art Meets Precision in Modern Advertising

römàn 1–20: Decoding the 20 Core Pillars Shaping Modern Innovation

